Anesthesiologists’ Best Practices: How to Succeed with Medicare PQRS and VBPM
 Anesthesiologists across the country are coping with a unique PQRS challenge. Different procedures and settings may mean that some practices do not have the requisite number of measures to meet requirements. Other groups will have enough measures, but the choices may not be obvious. When you have up to 6 percent of your Medicare Part B revenues at risk, you cannot afford to take that chance. Read on to learn how to make the best reporting decisions for your anesthesiology group and avoid Medicare penalties.
Anesthesiologists across the country are coping with a unique PQRS challenge. Different procedures and settings may mean that some practices do not have the requisite number of measures to meet requirements. Other groups will have enough measures, but the choices may not be obvious. When you have up to 6 percent of your Medicare Part B revenues at risk, you cannot afford to take that chance. Read on to learn how to make the best reporting decisions for your anesthesiology group and avoid Medicare penalties.
Like Orthopedists, your specialty focus inherently limits your relevant PQRS measures—except that for Anesthesia, the options are even more limited. In order to fulfill requirements, a specialist may need to report a measure with poor performance just to fulfill Medicare’s reporting requirements. Although this avoids a PQRS and its duplicate Value-Based Payment Modifier (VBPM) non-reporting penalty, reporting a measure with poor performance puts that provider at risk under the VBPM performance calculations.
Obviously, you want to avoid penalties for not reporting PQRS (which would trigger an automatic additional penalty through VBPM). Here are the basic reporting requirements: Individuals or groups who are reporting individual measures must complete nine measures for at least 50 percent of the eligible denominator, and those measures must include three National Quality Strategy Domains. One of those measures must be “cross-cutting,” a population-wide measure required for providers who see at least one patient in a “face-to-face” encounter, as defined by Medicare.
For Anesthesiologists, here are five steps to PQRS and VBPM reporting success:
Step 1: Understand the Measure Applicability Validation (MAV) Audit (or, Don’t Assume that Your Group Has Less Than Nine Measures)
Medicare recognizes that simply because two providers are of the same specialty, they will not necessarily render the same services. That is why measures are defined on a measure-by-measure basis, rather than by specialty. With that understanding, there is a provision for those who are unable to fulfill reporting requirements: the Measure Applicability Validation (MAV) Audit.
For those who report less than nine measures or less than three domains, Medicare will compare your claims to its measure specifications to see if there were any other measures where you or your group could have reported, but did not. Here’s the catch: these measures may not seem relevant to you, but they are to Medicare. This puts you at risk—you may believe (for example) that the patient’s Advance Care Plan is out of your realm, but Medicare won’t see it that way, and that would come out during the MAV Audit.
By working with a Registry that’s qualified to report on all measures, you should be able to see how you would fare in a MAV Audit. Aside from giving you protection from MAV, you can also see where you stand on the measures you are reporting.
In cases where it really does appear that you do not have nine measures or three NQS Domains available, you should contact the QualityNet Help Desk. They will review, and as a matter of course, provide email documentation of your discussion. While your situation may change, this documentation may be valuable should you need to request an informal review with Medicare.
Step 2: Report 2015 Measures Only (Skip #30)
As a Registry that has reported all measures across all specialties, we’ve seen our share of last minute client sign-ups. For these groups, one of the most challenging scenarios occurs when they see that a measure they had coded throughout the year was actually retired. Aside from the frustration over the wasted effort, the group must then scramble to find a substitute measure. This happens more than you may think. Medicare updates, adds and deletes measures each year, and specifications are released within weeks (or less) of implementation dates. In this period of transition and shuffle, not to mention how winter holidays can add to the challenge of keeping up with Medicare’s announcements at the end of the calendar year, things slip.
Case in point: In 2015, Medicare dropped the measure that was the mainstay of anesthesiologists: Measure #30, Perioperative Care: Timing of Prophylactic Antibiotic, Administering Physician. On page 744 of the Final Rule, Medicare addresses the reason for deletion, despite the pleas from PQRS participants:
Commenters disagreed with CMS’s proposal to remove this measure noting “it is premature to remove a measure based on a high-performance rate when the EP reporting rate within the PQRS program is low.” With a performance rate above 90 percent for multiple consecutive years, CMS considers the measure to have reached its potential, and no longer represents a clinical performance gap that should be measured by the PQRS Program. Additionally, CMS will apply the Measure Applicability Validation (MAV) process for claims-based reporting in those cases where specialists do not have enough relevant measures to report. For this reason, CMS is finalizing its proposal to remove this measure from reporting in 2015 PQRS.
To avoid a last-minute scramble, make sure that you are not counting Measure #30 as one of your PQRS measures.
Step 3: Capitalize on the Clinically Relevant Measures You Can Report
Anesthesia-specific measures are rare, and that means that you cannot afford to miss those available to you. Here are the most common:
- Patient Safety NQS Domain, Measure #193: Perioperative Temperature Management
- Patient Safety NQS Domain, Measure #76: Prevention of Central Venous Catheter (CVC) – Related Bloodstream Infections
- Effective Clinical Care NQS Domain, Measure #44: Coronary Artery Bypass Graft (CABG): Preoperative Beta-Blocker in Patients with Isolated CABG Surgery
As you can see, #44 is limited to coronary artery bypass grafts, and so it may not be possible to report this measure—even the measures identified as available for anesthesiology are limited!
In previous posts, we have addressed the importance of performance as it relates to your Value-Based Payment Modifier. With these measures, your performance is particularly important. With other specialties, there may be some variation (e.g. one cardiologist may report coronary artery disease measures, while another may focus on heart failure).
Anesthesiology does not have this flexibility, because most anesthesiologists will be reporting on a very small set of measures. Similar to what occurred with Measure #30, the fact that there are so few measures available means that practices have become hyper-focused on performing well, but it is difficult to distinguish yourself from the pack. Since these are process measures (outcomes are not considered), high performance rates are even more pronounced.
Fortunately, the specifications for these measures are relatively straightforward. The most important thing to remember is that these measures are to be reported for each instance, not for each patient. Don’t be lulled into thinking that the measure was completed and performed because you recorded it for a patient. Also, make sure that your documentation aligns with the 2015 version of the measure, including definitions (see Step 2, above).
Step 4: Remember Your Cross-Cutting Measure (Especially #47)
The “face-to-face” definition is not limited to office visits. Medicare has a list of “face-to-face” encounter codes, and they encompass nearly every specialty, including anesthesia. That means that a cross-cutting measure will likely be required for your practice.
The most frequently triggered cross-cutting measure we see on the anesthesiology side is Measure #47: [Advanced] Care Plan in the Communication and Care Coordination NQS Domain. We have learned from our clients that they were able to succeed in this measure by planning ahead. The hospital often has this information on record, and by checking beforehand, this can be added to your documentation, enabling you to report it to your Registry. Those who need to retrieve this information after the fact may have a more difficult time, as they cannot access hospital records from their offices.
Depending on who else practices with you and the types of services you provide, there may be other cross-cutting measures that apply. In the Patient Safety NQS Domain, Measure #130: Documentation of Current Medications in the Medical Record is common, as patients trigger this measure in many settings (not just ambulatory care). This stands to reason and is another good choice for anesthesiology. Few would argue that a provider, regardless of specialty, should be aware of a patient’s medication, particularly prior to administering a new medication.
Step 5: Look at All of Your Services—Do You Have a Pain Clinic?
The first thing we ask our anesthesiology clients is whether they have a Pain Clinic. Since Pain Clinics usually employ fewer providers and bill less expensive services, they are often overlooked when considering PQRS reporting. However, having a Pain Clinic is the single most important factor in determining how you will report for PQRS.
How can a small fraction of your providers and revenue make such a big difference in your reporting? It all comes back to which measures are available to your group, based on your services rendered. If you are reporting as a Group Practice, Medicare will look at anyone billing under your Tax Identification Number (TIN) who is considered an Eligible Professional (including nurses, physical therapists, occupational therapists and more). New and established patient office visits and PT/OT services will trigger dozens of measures on their own, including Preventive Care-based cross-cutting measures, most notably:
- #128: Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up
- #131: Pain Assessment and Follow-Up
- #226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- #317: Preventive Care and Screening: Screening for High Blood Pressure
In addition to these measures, others are triggered. They may not seem clinically relevant (e.g. cancer screening), or may seem too peripheral for reporting. Nevertheless, Medicare will see these as measures that you could have reported. The flip side is that you may have more clinically relevant measures than you realize, when looking at your entire group, and that opens up your options. You can report these to mitigate the risks described previously, whether related to measure completion or performance—just make sure that you are working within Medicare’s guidelines (your Registry should be able to help you here).
As an anesthesiologist, you may have a MAV Audit in your future. The best way to ensure that you pass—ensuring that you avoid PQRS and VBPM penalties—is to know where you stand beforehand. That means understanding your practice globally—minor nuances can mean major differences. However, a Registry doing comprehensive data capture and providing consultation services can help you ensure that you are ready for the audit, and perhaps bypass it altogether. You will be protected from the 6 percent penalty and positioned most advantageously for the Value-Based Payment Modifier.
Founded in 2002, ICLOPS has pioneered data registry solutions for improving population health. Our industry experts provide comprehensive PQRS Reporting with VBPM Consultation and ACO Reporting and Population Health Solutions that help you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session.
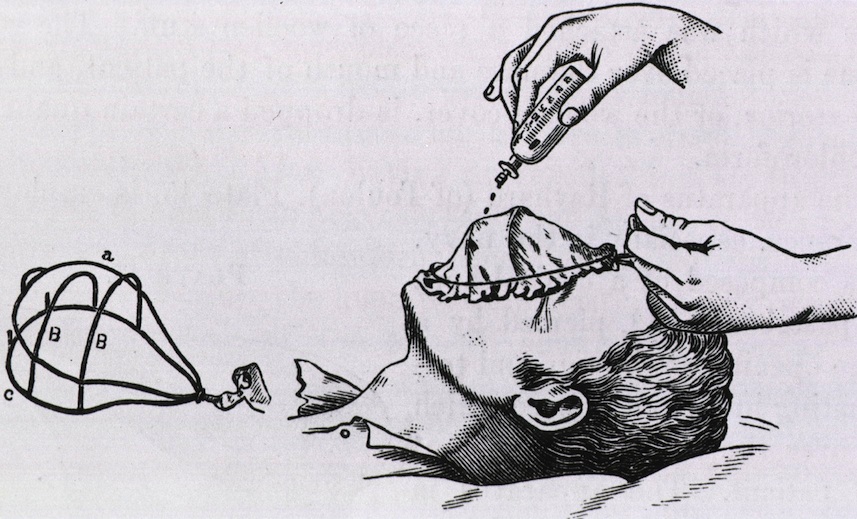
Image Credit: Modification Inhaler of Skinner and Charrier, of Paris, by Laurence Turnbull (1821-1900), Philadelphia: Blakston, 1896, National Library of Medicine