Who Else Cares for Your Patients? How the Wrong Patient Attribution Can Skew Your VBPM
 So, exactly who are your patients? Sounds like a silly question. But when it comes to Medicare’s patient attribution methodology, the answer is not obvious. Medicare attributes patients to providers and practices in order to calculate components of the Value-Based Payment Modifier (VBPM). Like it or not, certain patients can be attributed to your practice, even if their conditions are not under your clinical management, skewing your VBPM. If you don’t understand the rules, you risk significant penalties.
So, exactly who are your patients? Sounds like a silly question. But when it comes to Medicare’s patient attribution methodology, the answer is not obvious. Medicare attributes patients to providers and practices in order to calculate components of the Value-Based Payment Modifier (VBPM). Like it or not, certain patients can be attributed to your practice, even if their conditions are not under your clinical management, skewing your VBPM. If you don’t understand the rules, you risk significant penalties.
This is true for all providers, but most apparent in specialty groups. As a Qualified Registry and QCDR that reports all measures across all specialties, we’ve seen many cases where Medicare’s patient attribution varies considerably from how practices view the scope of their patient responsibility. Our analysis of Quality Resource and Use Reports (QRURs) from Medicare reveals to many clients they’ve been held accountable for outcomes outside of their realm.
A direct quote: “How can they penalize our orthopedists for a patient that was admitted for COPD?” Great question. Here’s how the calculations work and what actions you can take to protect your revenues:
How Medicare Attributes Patients for the Value-Based Payment Modifier
Medicare is shifting from Pay for Reporting to Pay for Performance through two programs: ACOs and the VBPM. Of the two, the VBPM is less clear—and less publicized, causing many providers to fall, unaware, into penalty status. Providers are being rewarded for providing higher quality care, while keeping costs down; those who do not, face penalties. Medicare quantifies quality and cost into two composite scores, using these to “tier” providers, compared to their peers.
The Quality Composite is based on two components:
- Performance rates on the measures you report for PQRS;
- Medicare-calculated claims-based outcome measures.
The Cost Composite is calculated by looking at costs for two groups:
- All Medicare Beneficiaries;
- Medicare Beneficiaries with at least one of four chronic conditions (Diabetes, Heart Failure, COPD, Coronary Artery Disease).
The PQRS portion of your Quality Composite should be very straight-forward, if you are receiving consultation services that review your prior QRURs and PQRS performance to determine on which measures to report. You should also have the ability to confirm which patients are included in your measures’ denominators, and why. In other words, the population under measurement is clearly defined, and you have the ability to monitor your status on an ongoing basis.
Attribution affects the remaining components. For the Quality Composite, Medicare analyzes its claims data to calculate outcomes for key indicators. This includes All Cause Readmissions and Ambulatory Care Sensitive Condition (ACSC) Admissions. For the Cost Composite, Medicare calculates the amount of spending per beneficiary, meaning all costs associated with the patient, whether you provided services or not. Here’s where the definition of “whose patient is whose” becomes crucial.
Attributions Depends on Who Provides “Plurality of Primary Care Services”
Medicare has a two-step process for determining which patients are tied to a provider and who will constitute the spending-per-beneficiary and claims-based-quality-measure denominators. Medicare aligns the ACO patient attribution method with the VBPM patient attribution, which creates consistency between Medicare’s Value-Based Payment initiatives. Just in case you did not make it to page 1030 in Medicare’s 2015 Final Rule, here’s how the attribution process works:
- Step 1: Beneficiaries are assigned to the primary care provider (whether physician, NP, PA, or CNS) who provided the “plurality of primary care services” to the patient, as measured by allowed charges. However, if the patient did not see a primary care provider . . .
- Step 2: Beneficiaries are assigned to the practice whose non-primary care providers (i.e. specialists) provided the “plurality of primary care services” to the patient, as measured by allowed charges.
“Primary Care Services” may include services that a specialist provides, but which are unrelated to the conditions and events that Medicare is tracking. Primary Care Services include (but are not limited to):
- For new patients—office or other outpatient visits, nursing facility care, domiciliary or rest home visits, or home visits;
- For established patients—office or other outpatient visits, nursing facility care, domiciliary or rest home visits, home visits, and discharge day management service.
To return to the earlier question: How can an orthopedic surgeon be penalized for a patient’s COPD admission or re-admission? If that patient with COPD did not see a primary care provider during the year, but did see an orthopedist in the office, the patient will be attributed to the orthopedic surgeon’s practice. If that patient gets admitted with a primary COPD diagnosis, the attributed provider is the orthopedist.
It makes no sense, but that’s how the calculations can work. Here are some ways to minimize your risk and ensure that you and Medicare are in sync:
Proactively Define Your Population to Protect Revenues
By understanding why your patients were attributed, you can take steps to ensure that you are being graded fairly.
- Analyze your QRURs for attribution patterns. Medicare provides feedback on attributed patients within the supplemental exhibits that accompany your QRUR. These exhibits provide patient-level details, including the names and NPIs of the providers (both in your group and out) who provided the plurality of primary care services. Studying which providers were attributed patients can provide insight on why patients were attributed. Some providers will have populations where this is to be expected; others may be surprised. For those who were not expecting to see attributed patients, how did it happen? Are there diagnoses or procedures that are more prevalent in your attributed patients?
- Track patients with diagnoses by another provider for one of the four chronic conditions. Both primary care providers and specialists can benefit from the information provided in the QRUR. Since it’s built from Medicare claims, the information is more comprehensive than what is available at the practice level. For example, a patient may have been hospitalized at an out-of-network institution. Medicare will see that through its claims, but that information may have never reached you. Similarly, other providers may have diagnosed patients with one of the four chronic conditions; you may not know that those patients, if attributed to you, are under extra scrutiny in the Medicare Spending Per Beneficiary model. It’s worth noting that QRURs show who was diagnosed in prior years, so providers may need to be more proactive to determine who was diagnosed this year (before getting an unpleasant surprise in next year’s report).
- Specialists should consider confirming whether their patients have a primary care provider, and whether they have seen him or her (or plan to) within the calendar year. Unfortunately, what’s sometimes lost within the nuances of attribution is that, when a patient is being linked to a specialist (rather than a primary care provider), it signifies a gap in care. When an orthopedist is penalized for a COPD admission, it means that no one is actually managing that patient’s COPD. By confirming that your patients, especially the ones with chronic conditions and who need ongoing care, are being managed by a primary care provider, you avoid this issue. With proper attribution, not only can you avoid VBPM penalties based on their costs, but also those patients can be appropriately treated. This means better outcomes all around.
- Ensure that your successful patients are properly attributed to your practice. There’s a flip side to the attribution coin, and primary care providers should take note: if there is more than one primary care provider, Medicare will look for the one who provided plurality of primary care services, based on charges. Physicians who have worked with patients for years to quit smoking, bring their blood pressure in control and start exercising need to be sure these patients are going to be attributed to them so they can demonstrate good outcomes. This sounds obvious, but the playing field is rapidly changing, with some significant consequences.
Specifically, large retailers, including Wal-Mart and Walgreen’s, have formed ACOs. Their clinic nurses provide “primary care services,” and for a variety of reasons, they may provide the “plurality” of these services for patients. The business model for these retailers’ ACOs is tied to attribution—they believe that, by maintaining frequent contact with patients and ensuring they have access to medication and other treatment, they are able to keep their patients’ healthcare costs down. They can siphon off the physician’s easier cases (the patients less likely to require hospital care or experience complications), and refer back the complicated ones—the patients with chronic conditions who are more likely to be at risk. So, while a patient may see his or her primary care physician each year (and receive a clean bill of health), that doesn’t guarantee that the healthy patient will be factored into that provider’s VBPM. One activity to consider is the inclusion of a Medicare Wellness Visit for your primary care patients; the provision of that service weighs into Medicare’s calculations of who is the attributable primary care provider.
The lesson here is simple: Whether you are a primary care provider or a specialist, you need to know what care your patients are receiving, even after they leave your office. You no longer have the luxury of providing the best possible care in your field and sending patients on their way. In the Pay for Performance environment, whether ACO or VBPM, your performance on quality and cost metrics are defined patient-centrically—and that can mean payment based on what’s been done (or hasn’t) after the patient has left your office, regardless of whether it’s within your control.
Founded in 2002, ICLOPS has pioneered data registry solutions for improving population health. Our industry experts provide comprehensive ACO Reporting and Population Health and PQRS Reporting with VBPM Consultation Solutions that help you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session.
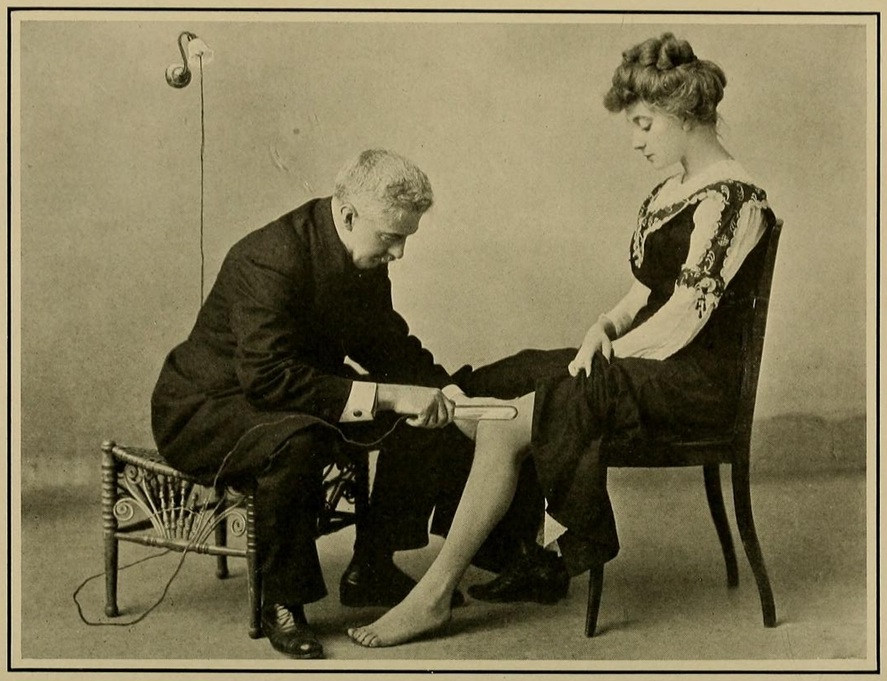
Image Credit: “High Frequency Electric Currents in Medicine and Dentistry (1910)” by Samuel Howard Monell, courtesy of The Public Domain Review.