Final PQRS 2015 Reporting Rule: Higher Penalties and Tougher Requirements
 Looking for a good bedtime read? CMS has finalized its 1200-page Medicare Physician Payment System rule for 2015. While the full version is a sure cure for insomnia, buried within are two areas worth your attention: 2015 PQRS Reporting, and Medicare’s Value-Based Payment Modifier (VBPM). Central to Medicare’s value-based health care efforts, both impose stiffer penalty risks for physician groups in 2015.
Looking for a good bedtime read? CMS has finalized its 1200-page Medicare Physician Payment System rule for 2015. While the full version is a sure cure for insomnia, buried within are two areas worth your attention: 2015 PQRS Reporting, and Medicare’s Value-Based Payment Modifier (VBPM). Central to Medicare’s value-based health care efforts, both impose stiffer penalty risks for physician groups in 2015.
Here are key rule highlights for these two programs, modified slightly from the proposed rule.
Higher Penalties for PQRS Non-Reporting
- Failure to report PQRS triggers two penalties: a PQRS non-reporting penalty of 2 percent, plus a VBPM non-reporting penalty ranging from 2 to 4 percent.
- All groups are subject to BOTH non-reporting penalties, regardless of size. However, the VBPM penalty is keyed to group size: 2 percent for groups of under 10, and 4 percent for those 10 or over. This is double the 2014 rate for almost everyone.
Higher Bar to Avoid PQRS Non-Reporting Penalties
- There is no longer a “safety net” of minimal reporting to avoid a penalty; 2014 three-measure reporting has been eliminated as an option.
- There is no PQRS bonus for 2015 reporting.
- Groups reporting individual measures, or those reporting under the Group Reporting Option (GPRO) and with fewer than 100 providers, must report 9 measures in 3 “Domains” of care, with 50 percent completion of measures for all eligible patients.
- One cross-cutting measure is required for Registry Reporting for all providers who see at least one Part B patient in a face-to-face encounter. These are often called “population health” measures and include services such as tobacco use assessment or depression screening. Not all registries will be qualified to report these measures.
- GPRO-reporting groups with 100 or more providers must report CAHPS measures, plus 6 measures across 2 domains, one of which must be a cross-cutting measure.
- Important measure changes include deletion of commonly used measures such as peri-operative antibiotic timing measures, some stroke measures, the asthma assessment measure and non-ER diabetes lipid tests. Current Emergency Room measures are being deleted, and some measures have become Registry-only.
- Reporting methods remain the same overall, although there are restrictions for how some groups may report and which measures may be reported through each method:
- Registry Individual or Group Reporting Option (GPRO) or Measures Groups
- Qualified Clinical Data Registry (QCDR)
- EMR Direct
- GPRO Web Interface
- Administrative Claims
- GPRO Reporting has a June 30 self-nomination deadline, three months earlier than 2014.
Incentives and Penalties under the Value-Based Payment Modifier
- Quality-tiering formula remains generally equivalent to 2014 regarding components and the construction of Quality and Cost Composites.
- Quality tiering will be imposed on all groups, with these conditions:
- Groups from 1 to 9 providers will not be subject to any penalties based on 2015 results.
- Groups of 10 or more are subject to incentives up to +4 percent or penalties to -4 percent of 2017 Medicare revenues, based on quality tiering results—even with PQRS reporting requirements met.
- Groups/practices comprised exclusively of non-physician providers are excluded until 2016.
- ACO providers will be eligible for the VBPM quality component, unlike earlier years. Providers in Pioneer ACOs or a CMS Clinical Performance Measure project will still be exempt.
- Quality tiering maintains important features:
- Ambulatory-sensitive admissions will continue to fall into the Quality composite.
- PQRS Measure selection still features heavily into the quality tiering results. Individual measure reporting has a new feature that will weigh performance rates for all reporting providers. This raises the possibility that one provider could negatively impact the whole group, depending on the measures used by that provider.
- For providers reporting through a QCDR, the tiering will be neutral if CMS cannot calculate a quality composite.
- The minimum number of admissions in the “All Cause Re-admission” measure is increased from 20 to 200.
- Cost tiering formula has one important expansion:
- Attribution of costs to providers will now include visits with NPs/PAs in a group. If there is no primary care provider, cost is attributed to the plurality of primary care services (measured by allowed charges).
- Part-year beneficiaries are included the total costs.
Founded in 2002, ICLOPS has pioneered data registry solutions for improving population health. Our industry experts provide comprehensive PQRS Reporting with VBPM Consultation that helps you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session.
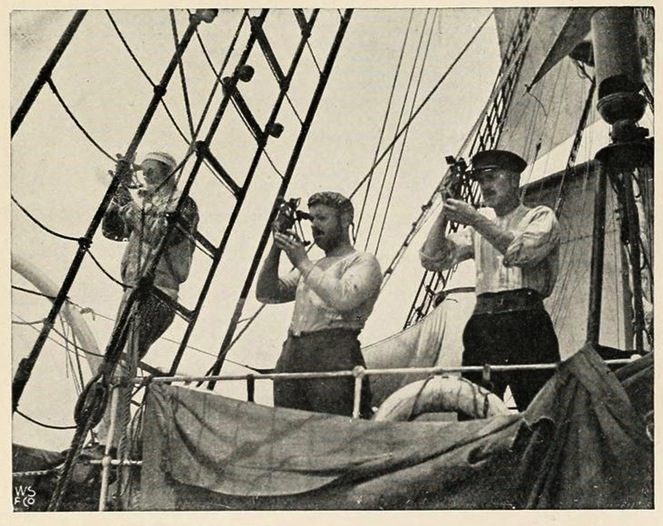
Image Credit: “Taking an Observation,” from The South pole; an account of the Norwegian Antarctic expedition in the “Fram,” 1910-1912, by Roald Amundsen, University of Toronto Libraries. See more at Public Domain Review.