Medicare Is Playing by 2015 Rules—Are You?
 Does it feel like 2015 yet? While we may fill out paperwork that reads “2014 2015” for the next few weeks, 2015 is here—and it’s different. Do you need evidence? The 2015 Medicare Physician Fee Schedule is officially in effect.
Does it feel like 2015 yet? While we may fill out paperwork that reads “2014 2015” for the next few weeks, 2015 is here—and it’s different. Do you need evidence? The 2015 Medicare Physician Fee Schedule is officially in effect.
Several hundred pages within the 1200-page “Final Rule” describe the rules for the 2015 Physician Quality Reporting System (PQRS) and the 2017 Value-Based Payment Modifier (VBPM). Make no mistake—there is no transition period; these rules are in place today whether you’re ready or not.
So, now that we’re playing by 2015 rules, what do you need to know?
PQRS 2015 Is Now Mandatory with No Safety Nets—Know the Requirements
PQRS is mandatory, and you must meet the full reporting requirements to avoid a penalty (there is no longer a PQRS bonus). In previous years, there were “safety nets” that enabled providers to meet intermediate requirements; they would not earn an incentive, but they were protected from penalties. That is no longer an option.
There are different reporting methods, and requirements differ by type of reporting and by the size of your group. Here is what’s required in 2015 for practices that utilize the Group Practice Reporting Option (GPRO) through a registry (don’t forget to submit to CMS for GPRO Registry Reporting by June 30, 2015!):
- For groups of 100 or more providers:
- You must report a minimum of six measures, completing each measure on at least 50 percent of eligible patients.
- Those six measures need to represent two of the possible six National Quality Strategy (NQS) Domains.
- For any group with even a single “face-to-face” encounter, at least one “cross-cutting measure” must be included in the measure sample. These measures are designed to apply across the spectrum of care, including topics such as immunizations, preventive care and lifestyle.
- Administer (at your expense) the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey, and report the results. This survey is counted in lieu of three additional PQRS measures
- For groups of 2 to 99 providers:
- You must report a minimum of nine measures, completing each measure on at least 50 percent of eligible patients.
- Those nine measures need to represent three of the possible six National Quality Strategy (NQS) Domains.
- The same “cross-cutting” measure requirement applies as for larger groups. To clarify, this measure can be counted as one of your nine measures; you do not need to report nine measures and an additional “cross-cutting” measure.
Providers using a Registry and reporting individually (either within a group or as a solo-practitioner) can either report using individual measures or a measures group. Individual measure requirements are the same as for groups with 2 to 99 providers. Measures groups are CMS-defined sets of individual measures related to a specific condition or procedure (e.g. Diabetes or Total Knee Replacement). A provider must report each component in the group for a minimum of 20 patients, 11 of whom must be Medicare Part B.
Please note: Groups can report as a collection of individuals, but at least half of the providers must meet PQRS requirements. Otherwise, the whole group will be penalized under VBPM, in addition to the non-reporting PQRS penalty that will follow those who did not succeed.
Choose Reporting Method Carefully—Not All Measures Can Be Reported with Each Method
In addition to Registry Reporting, other methods of reporting PQRS to Medicare are available:
- EMR-Direct
- Administrative Claims
- GPRO Web Interface (direct entry into CMS website)
- Qualified Clinical Data Registry (QCDR)
Remember, not all measures can be reported using these methods, and program requirements may vary. The first three (EMR Direct, Claims, the CMS Web Interface) appear easier, but you lose control of your quality composite and therefore risk being penalized under the Value-Based Payment Modifier. This is because you can’t select your measures or the patients included in your reporting sample, and so your results will be determined by CMS calculations, and can’t be improved by you.
The final option (QCDR) may be more challenging, as it requires reporting on all patients (not just Medicare), but it offers a unique opportunity to improve quality across the practice while fulfilling reporting requirements. See our previous blogs on why it’s dangerous to give up control of your quality composite, and who may benefit from a QCDR.
PQRS 2015 Reporting Failures Bring Higher Penalties—Four Times Greater in 2017
If you do not fulfill PQRS reporting requirements in 2015, you can expect to receive a letter from CMS informing you that your reimbursement will be cut by 2 percent for not reporting in PQRS, plus an additional 2 percent or 4 percent (groups under 10 or with 10 or more providers respectively) for the Value-Based Payment Modifier. Many were stunned to receive CMS’s 2014 notice that their rates would be cut 1.5 percent; the next letter will hit harder—the amount at stake in 2017 (based on 2015 services) is four times greater.
The Value-Based Payment Modifier is tied to, but separate from, PQRS. VBPM is Medicare’s move to pay-for-performance, rewarding high-quality and low-cost providers with the penalties levied on low-quality and high-cost providers. In other words, you’re in competition, and the losers pay the winners. (To learn more, see our free Resource Guide, How to Minimize Risk Under the Value-Based Modifier: 10 Essential Facts About CMS Quality Tiering.)
PQRS Reporting Rules Are a Moving Target—Stay Informed About Updates
Finally, a warning to those who are poised to succeed in the 2014 PQRS program: don’t be lulled into thinking that you have 2015 covered! Each year, Medicare changes measures within PQRS. Some are added, others are retired, and some are edited to include (or exclude) certain patients. That is all true again for 2015, but there is now an additional wrinkle: some measures are being moved from one NQS Domain to another. Pay attention to the 2015 changes so that you’re not among the panicked practices in December 2015 who are scrambling to fix a problem caused by reporting a measure that CMS no longer recognizes, or that no longer covers the same NQS Domain that it did in 2014.
So, what can you do? Start now. Determine how you want to report for PQRS based on what’s important to you. Is it ease or control? Do you simply want the tools for meeting minimum requirements or a partner who will work with you to excel? Only you can make these choices, and you should make them quickly. How you report will affect what measures you have available; Medicare has already started calculating who is eligible, and unless you’ve been reporting by 2015 rules, you may already have to catch up. PQRS has become a more comprehensive and challenging endeavor, and with the incorporation of the VBPM, PQRS penalties are only a taste of what’s to come.
Founded in 2002, ICLOPS has pioneered data registry solutions for improving population health. Our industry experts provide comprehensive PQRS Reporting with VBPM Consultation that helps you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session.
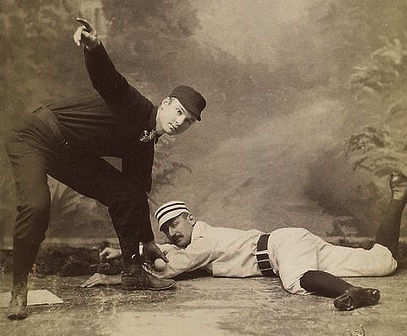
Image Credit: “Posed Portraits of 19th Century Baseball Stars” from the New York Public Library’s Spaulding Collection; photo by Gilbert & Bacon, Philadelphia, circa 1870-1880; courtesy of The Public Domain Review.