Don’t Miss GPRO Deadline: Choose (and Register) by June 30
 For many, June 30 means the fiscal year is coming to its end. It also means the deadline for self-nominating for the Group Practice Reporting Option for PQRS looms near. Why does it matter? Because your selection (or lack thereof) has the potential to substantially impact your budget in 2018, and the GPRO registration deadline is June 30.
For many, June 30 means the fiscal year is coming to its end. It also means the deadline for self-nominating for the Group Practice Reporting Option for PQRS looms near. Why does it matter? Because your selection (or lack thereof) has the potential to substantially impact your budget in 2018, and the GPRO registration deadline is June 30.
Millions of dollars are at stake. Failing to report for PQRS means that CMS will hold back 6 percent of all Medicare Part B reimbursements in 2018—a 2 percent penalty for not reporting PQRS, plus a 4 percent penalty for the Value Modifier for groups with 10 or more providers.
On the other hand, reporting successfully and demonstrating significantly better performance than peers can mean an incentive payment under the Value Modifier, and it can be substantial—in 2016 (based on 2014), ICLOPS has clients earning incentive payments from about 16 percent to nearly 32 percent on the same Part B reimbursements—a potential swing of almost 38 percent!
Get used to numbers like this. With MACRA and the Quality Payment Program (QPP, which includes MIPS) just around the corner, preparing for and succeeding in PQRS and the Value Modifier positions you for significant gains. So, what choice should you make now (or by June 30, latest) to protect your organization today while simultaneously preparing for the future?
Your GPRO Registration Options
There are four reporting options when registering your Group Practice:
- Qualified Clinical Data Registry (QCDR)
- Registry
- EHR-Direct
- Web Interface
1. Qualified Clinical Data Registry (QCDR)
The QCDR option for Group Practice reporting is new for 2016 (previously limited to individual providers). This intriguing option enables you to fulfill PQRS requirements using non-PQRS measures.
Many specialty providers lament lack of available measures for PQRS and having to report something irrelevant simply to “get the job done.” But if quality reporting were to play a meaningful role in a larger quality improvement strategy and also provide more meaningful measures, you would have a win-win. That’s the purpose of the QCDR—not to act simply as data middleman, but, rather, to facilitate improved outcomes. It provides an active mechanism to deliver high quality care, confirmed through measurement.
The Proposed MACRA Rule, which lays the groundwork for the QPP and MIPS, has cleared a pathway for QCDRs to fulfill a variety of requirements in the post-PQRS world. QCDRs can be used to improve MIPS scoring in Quality, Clinical Practice Improvement Activities or Advancing Care Information; leveraged to strengthen your overall quality strategy; and may positively impact your Resource Use score down the road.
QCDRs require 9 measures across 3 NQS Domains, but also require outcome measures as well as reporting on all patients (not just Medicare Part B). While some providers may decide against a QCDR option because this reporting approach involves all patients (and therefore possibly more work), the Proposed Rule will apply quality measures to all patients anyway, under MIPS/QPP. Discarding this option now may mean that you are unprepared for 2017.
Review CMS’s list of approved QCDRs to see which offer measures designed to engage providers—not administrative or IT staff—in performance improvement.
2. Registry
There were few changes to the Registry Reporting option for Group Practices from 2015 to 2016, which may make using this option easier. The requirements are the same—report on 9 measures for at least 50 percent of eligible patients, including a cross-cutting measure, and make sure your measures represent at least 3 National Quality and Strategy (NQS) Domains. Only Medicare Part B patients are included.
Both Registry reporting and QCDR reporting give your organization the opportunity to align your Quality efforts. Since the Value Modifier is calculated using all measures reported in PQRS, reporting as individuals can quickly diminish your ability to control your composite. For example, if one provider reports 9 measures and another also reports 9, but only 2 of those measures overlap, suddenly you’re being scored on 17 measures. Add more providers, and your control decreases exponentially. It is also difficult to administer. There are forms to be signed for each provider reporting as an individual (not as part of a Group Practice), and those on the management side are tasked with ensuring that no one falls through the cracks.
On the other hand, with Group Practice reporting, the group can align around a specific set, creating a common goal, and ensuring that you’re being scored according to your strategic selections. The right Registry or QCDR will help you through this process.
3. EHR-Direct
Many practices choose to have their EHR simply report the measures to CMS, opting to avoid the step of sending data elsewhere. Since EHR functionality in PQRS varies considerably, make sure that simplicity is not going to cost you later. Here are some criteria to check before deciding that your EHR is a good choice:
- Do you have access to ongoing performance results by measure and comparisons with other providers?
- Does your EHR support a limited or the broadest span of measures available?
- Most important for identifying “your” best measures, does your EHR report all measures with data, or can you select those where your performance is higher than the CMS Mean (and does the EHR provide this data)?
- How does your EHR transition its technology from performance measurement to improvement?
- How current is the coding structure used by the EHR to update PQRS or other measurement values?
Answers to these questions will help you determine whether the convenience of the EHR reporting is worth more than the potential performance-based penalty you may achieve under the VM. Since PQRS and your future experience under MIPS and APMs are highly determined by comparison of your performance on quality and cost with others, it makes sense that you use the tools that will get you there fastest.
4. Web Interface
This method is strictly between the group and CMS. At the end of the year, CMS will provide these practices with a list of patients who must be reported for a pre-defined set of primary-care focused measures. The list is ranked, and groups must report consecutive patients, from 1 through 248. It is possible to skip a patient, but only under certain circumstances (e.g. medical record not available). All other patients are fair game.
Although this method is the most straightforward, you lose any chance to steer your Quality Composite beyond hoping that your healthiest patients have been selected in CMS’s sample. In practice, you may have a high number of patients with well-controlled blood pressures, but if those patients are not included in the sample (or are included, but ranked far enough down the line that they are not reported), they do not help your Quality Composite. Only those that are in the reporting sample (and reported) will be used by CMS to determine your Quality Composite. So you’re taking a big risk that your hypertensive patients with 120/80 values are well represented, and the 200/150 group is not in the sample.
For groups with at least 25 providers, the CMS Web Interface is the sole way to report with only internal resources. Your staff will be tasked with manually reviewing charts and entering responses into CMS’s web portal. In addition, you must be willing to trade your Quality Composite and public quality standing (on Physician Compare) for keeping your effort in-house.
Frequently Asked Questions
Once you’ve determined how to report, it’s important that you make your selections before the June 30 window closes. To prevent you from getting stuck before the finish line, here are some questions (and answers) we’ve been fielding since CMS opened its portal:
We have not finalized the agreement with our Registry/QCDR—can we still register?
Even if you haven’t picked a Registry yet (let’s hope you’re in the final stages of your decision), you can register as a Group Practice. You do not need to declare with a specific vendor, so if you’ve decided on Registry Reporting, there’s no need to wait, and in fact, you probably shouldn’t. The June 30 deadline is not flexible; if you’re stalling until your agreement is signed before you register, your group’s ability to report as a group and optimize its VM quality composite may be derailed by a single missed email or one person’s vacation.
We have not picked measures—can we still register?
You also do not need to pre-select measures. Reporting as a Group Practice through a CMS-qualified Registry or QCDR gives you the opportunity to pick and choose (within the confines of PQRS requirements) which measures you would like to report—a good Registry or QCDR partner will help you with this—but you don’t have to declare them advance. So, even if you’re on the fence about whether to pick one measure or another, or want to see if you can improve your performance on a specific measure before deciding, you are free to register.
What about the “CAHPS for PQRS” Survey?
When registering as a Group Practice, in addition to selecting a reporting mechanism, you will need to determine whether to include the CAHPS for PQRS survey in your VM Quality Composite. First, a caveat: if your group has 100 or more eligible professionals, the survey is mandatory, and you are responsible for selecting a qualified survey vendor and for the costs of the survey. But you are not required to include the survey results in your Quality Composite—you only need to decide whether or not to include them.
If you include the results, it means you have fewer measures that you need to report—6, rather than 9, and 2 NQS Domains, rather than 3. In exchange for reporting fewer measures, you cede a degree of control of your quality scoring to those survey results. CMS will notify your survey vendor who is eligible, based on the patients attributed to your group through CMS’s attribution process (driven by who is providing primary care services to your patients). Your survey vendor will distribute and score the survey, then send the results to CMS. You are completely removed from the process. So it comes down to this: Are you comfortable with your patient satisfaction scores being used to dictate your quality composite and 2018 reimbursement?
A Final Word of Caution—and Some Helpful Resources
GPRO Registration is required yearly. Don’t fall into the trap of thinking that just because you reported this way last year, you’re doing it the same way this year. Also (we’ve seen this), don’t assume that “someone” has handled the registration. If you don’t know who did it, verify. Don’t find yourself scrambling to answer a question about GPRO registration on July 1.
For more information on each of these reporting methods, see these official CMS documents:
- 2016 QCDR Reporting Made Simple
- 2016 Registry Reporting Made Simple
- 2016 GPRO Web Interface Made Simple
Founded in 2002, ICLOPS has pioneered data registry solutions for improving patient health. Our industry experts provide comprehensive Solutions that help you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session
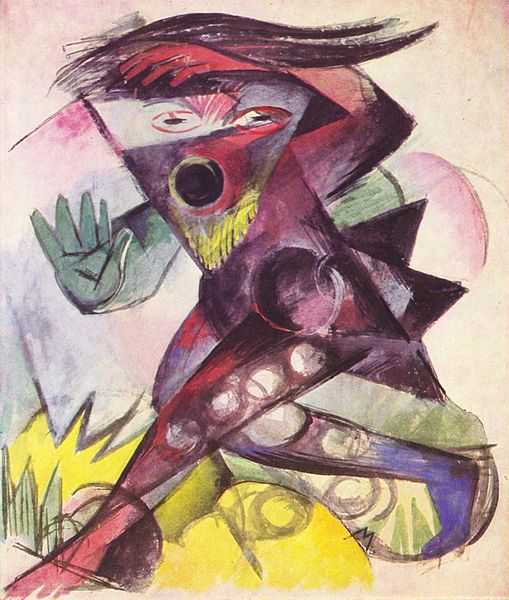
Image Credit: Caliban, Figurine für Shakespeares “Sturm” by Franz Marc, 1914; The Yorck Project: 10.000 Meisterwerke der Malerei. DVD-ROM, 2002. ISBN 3936122202. Distributed by DIRECTMEDIA Publishing GmbH. U.S. Public Domain.