For ACOs to remain relevant and viable under risk payment models, they must step up now to generate more cost savings for Medicare patient care. Medicare’s budget cuts are once again under consideration as political pressure mounts to lower governmental spending. CMS is expanding risk through Medicare value-based payment models, such as the new ACO PC Flex model, which is designed to create per-patient reimbursement for small ACOs in trade for higher reimbursements and funding for infrastructure. Most newer CMS payment models are now incorporating per-patient payments designed to lower the total cost of care.
As the provider-driven vanguard in the Medicare Value-Based Care effort, ACOs’ total savings represent just slightly over 1 percent of $944.3 billion in total Medicare spending. Some ACOs have individually generated higher savings for their patients’ care, but others are at zero or in the red. ACOs collectively produced a considerable $10.5 billion in savings in the most recent reported year of 2022. But it is not enough to forestall budget cuts in the program as the fiscal situation tightens.
Why just one percent? The answer isn’t complicated: The way ACOs try to reduce costs is, in most cases, not sophisticated enough. And they have lacked the tools to save more.
Soft Sell on Costs in Value-Based Care—Until Now
Cutting costs in health care is fraught with misperceptions, starting with the notion that cost control invariably hurts patients. Those misperceptions have emerged from experience with cost management through prior authorization and benefit cuts by payers and payer-providers. From its inception, the ACO model emphasized that lower costs would automatically result from better coordination of care and improvements in patient health.
ACOs’ pursuit of population health strategies to reduce hospital admissions and emergency room visits did produce some savings. ACOs also went after low hanging fruit to reduce costs, such as skilled nursing facility stays for the maximum time frame rather than for the patient’s actual therapeutic needs. But the totals tell the story— the savings from these basic approaches are not enough and won’t be enough to ensure the future of ACOs.
Unfortunately, cost control is never “automatic.” It requires measurement, understanding and ferreting out cost drivers, cost variation, and other exacting elements of cost.
Escalation in health care costs involves many hidden factors—practice patterns, patient engagement in initiatives to improve health, equitable access and services, and the slow and certain progression of chronic disease and risk factors into more serious and costly illness. Note that many of these factors involve clinical factors and patient-physician communication during care delivery. Addressing these issues will help, not hurt, patients.
Many of the highest costs are incurred from specialty care diagnostics and treatment. But many ACOs have considered specialty care beyond their purview, by virtue of both the reimbursement system and their membership makeup.
Bootstrapped ACOs Have Lacked Data and Tools for Cost Control
Measurement and successful cost control strategies require data. Until recently, most ACOs received quarterly retrospective data from CMS for their patient services. But not all used even this transactional data. Apart from diagnosis information and events, claims data does not contain the clinical information needed to ascertain patient condition or risk level. Thus, population health cannot identify the highest risk individuals except by counting events and comorbidities associated with claims. There is little predictive capacity in this data.
Since the drivers of cost are clinical, ACOs also need clinical data from their participating physician groups’ EHRs to adequately pursue cost control strategies and identify the drivers in cost variation.
In the last year, CMS rules have put greater emphasis on ACO aggregation of data, by way of two new requirements. First, the transition in ACO quality reporting from sample-based reporting to APP Reporting pushes ACOs to begin taking data aggregation seriously in order to perform APP reporting successfully. Second, the recent Quality Payment Program rule changes require ACOs to facilitate a transition of their participating practices to Certified EHRs, making it easier for data aggregation.
It won’t be long before ACOs are no longer data-impoverished and will have the means to pursue real cost control in conjunction with clinical excellence and outcomes for patients. But to accomplish that, they’ll need a strategic map.
How to Develop a Strategic Map for Cost Control
ACOs will need a number of concerted strategies designed to pursue better patient care and outcomes; many of those strategies will involve linking quality and patient treatment to cost consequences. For those new to EHR data, this is complicated territory. Your ACO needs to know how to navigate data quality, data gaps, priorities for your patients, priorities for the ACO, your physician involvement, and how to evaluate costs.
At Roji Health Intelligence, we’ve been evaluating clinical information and turning it into cost- and value-based strategies for more than 20 years. We have created a template for ACOs embarking on this journey and are introducing this series to help you navigate the development of initial and ongoing strategies. Over the next several articles, we’ll delve into how to launch cost control with a clinical focus.
First up, what you can accomplish using your most readily available data, and how to expand capabilities once data is aggregated on a larger scale. In future articles, we’ll present strategies for collaborating with specialists, assess Artificial Intelligence tools, and discuss what you must know as you embark on this mission. We hope you’ll share this with your colleagues and take the needed steps now to help your ACO flourish.
Founded in 2002, Roji Health Intelligence guides health care systems, providers and patients on the path to better health through Solutions that help providers improve their value and succeed in Risk.
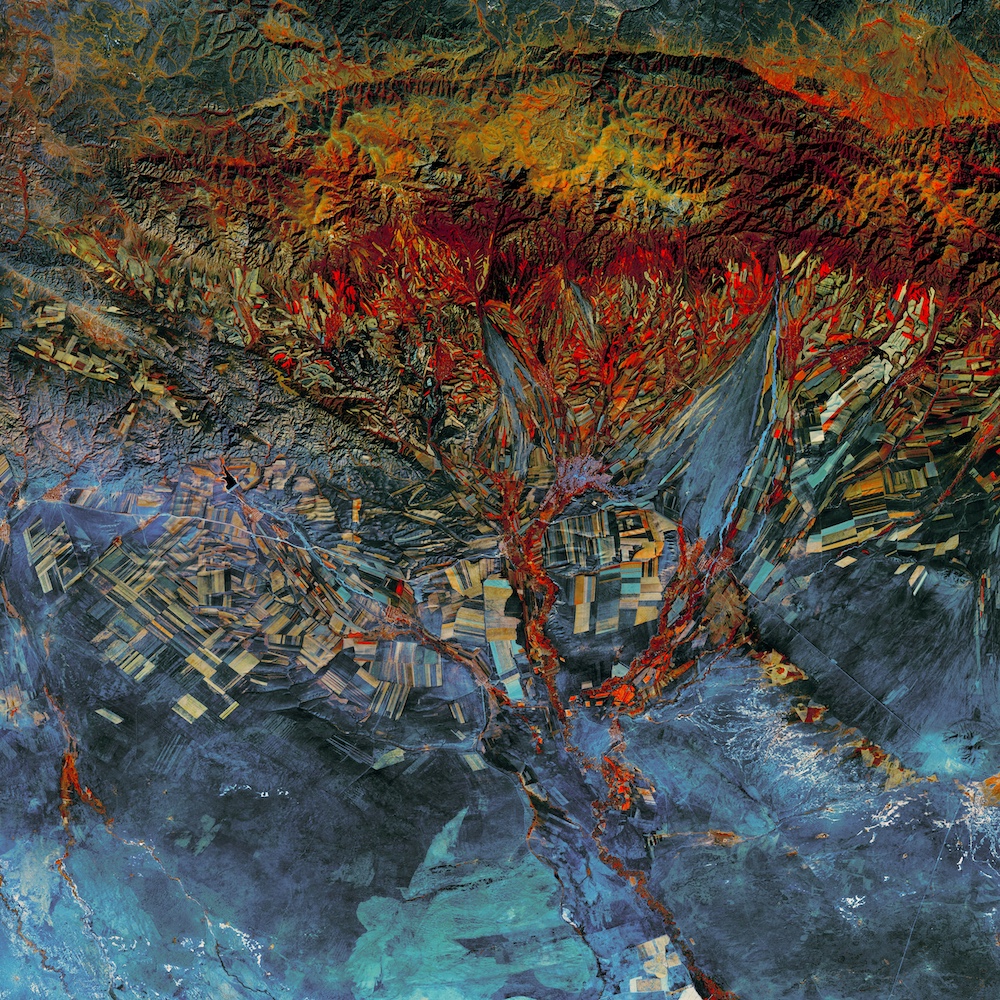
Image: USGS
