The CMS TEAM payment model focuses on the patient surgery and recovery process, which puts hospitals at risk for both cost and quality of surgeries. The end result of TEAM, if implemented well by hospitals and clinicians, is benefits for patients, with more coordination of services and fewer complications. The American College of Surgeons supports […]
Rethink the Essential Role of Primary Care Physicians in TEAM
With TEAM’s focus on improving surgical recoveries and costs in major hospital-based surgeries, it’s easy to miss the importance of primary care physicians. But their role is essential for meeting TEAM’s objective to improve patient recovery and lower costs in the five major types of surgery covered by TEAM. And perhaps not in the way […]
New TIPS for TEAM: Adopt ERAS Guidelines for Prevention of Complications and Faster Recovery
If TEAM has your hospital searching for an evidence-based toolkit to improve surgical outcomes and reduce recovery time, participating hospitals and their surgical teams should pay heed to ERAS (Enhanced Recovery After Surgery) protocols. The guidelines are tailored to more than twenty types of surgery as well as anesthesia and intensive care. They have been […]
TIPS for TEAM: How to Reduce the Top Driver of Higher Variable Costs in Surgery Episodes
One of the largest and most significant changes to specialty care payments in Medicare commences in January. TEAM (Transforming Episode Accountability Model) is poised to put hospitals at risk for total costs of care for the highest cost Medicare surgical episodes, including Coronary Artery Bypass Graft (CABG), Lower Extremity Joint Replacements (LEJR), major bowel procedures, […]
The 2026 CMS PFS Final Rule: The 5 Ways CMS Aims to Control Total Cost of Care
The CMS PFS Final Rule is out . . . early? If you’re wondering how, in the midst of the Shutdown, a 2,375-page Rule could be released, the answer is simple: most of the proposals from this summer were finalized as is. There are always exceptions, but the big takeaway is that this Rule solidifies […]
Three Strategies for ACOs to Optimize Specialty Care through TEAM
Both the greatest strength and weakness of the ACO shared savings (MSSP) model is its focus on primary care, particularly chronic disease. ACOs have put patients with diabetes, hypertension, and other conditions usually handled through primary care physicians at the center of care coordination, population health, and care management. But as CMS Value-Based Care’s central […]
CMS is Demanding Change in Specialty Care: 5 Things to Know about ASM
Heads up! CMS’s Proposed 2026 PFS Rule introduces a new payment model for tackling specialty care and costs in traditional Medicare. Clearly not a snap decision, Ambulatory Specialty Model (ASM) has been cooked until well-seasoned and served up in 210 pages of the proposed Rule. Unlike a typical Notice from the CMS Innovation Center that […]
CMS Commits to Control Total Cost of Care: 6 Volleys in the 2026 CMS PFS Proposed Rule
Summer is here, and the heat is on: barbeques, beaches, and the 2026 CMS Physician Fee Schedule Proposed Rule. Throughout 1,803 pages, CMS is going after the total cost of care in the MIPS and APM tracks of the Quality Payment Program (QPP). These proposed updates and the creation of a surprise new (and mandatory!) […]
Roji Health Intelligence Response to CMS RFI for Health Technology Ecosystem
Data and technology, once simply functional assets to facilitate health care, are now a leading force for health care advancement, improvement of health care outcomes, and control of costs. Yet the panoply of technologies has not optimized information for one key actor: the patient. The Center for Medicare and Medicaid Services (CMS) is attempting to […]
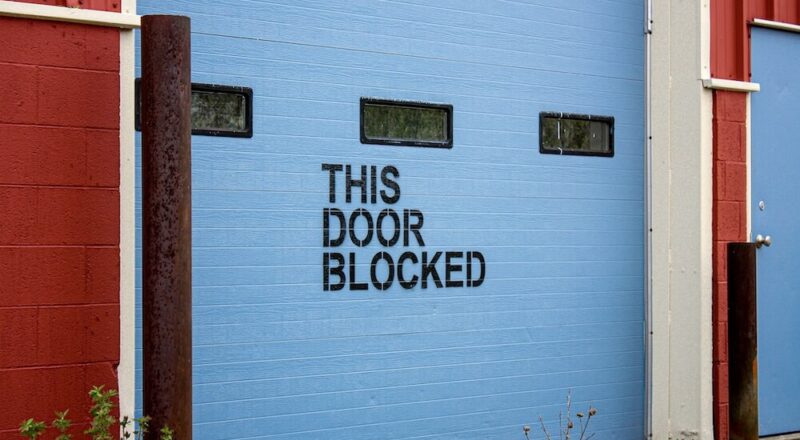
Let’s Put an End to What Blocks Providers and Patients from Controlling Health Care Costs
We often blame providers for not controlling health care costs. We also put the onus on patients who overuse care inappropriately and make bad choices. But the fact is that control of health care costs is extremely complicated, and we have effectively blocked both providers and patients from controlling health care costs. Since the birth […]