Health care technology (HIT) is frequently oversold. That may be a surprising message coming from a Registry CEO, but it’s the truth. In the quest for answers, too many providers search for a system that can “do it all,” a dream technology that exists, well, only in your dreams.
There is intense pressure on providers to prepare for undertaking the financial risk of patient care, while maintaining or improving patient quality and outcomes. Two factors are driving the push for HIT purchases to meet this demand: providers’ strong wish for easy and straightforward solutions that can mesh with existing technology, and technology vendors’ desires to sell more products to their current customer base and increase revenues. Indeed, technology vendors have successfully convinced providers to connect systems, use analytics and expand the use of their EMRs.
Technology Differences Defined by Areas of Excellence
Like every other technology, however, from accounting to telecommunications, the One-Stop Solution is a myth. Here’s why:
- Different technologies have unique functionalities and distinctions. When you have a specific area of medical concern, like your heart, you see a cardiologist, because that physician has the expertise you seek, experience and access to the latest body of knowledge. The same goes for technology—most health care technologies arose from specialized knowledge, and these technologies keep abreast of developments within their areas of specialization. In Performance Measurement, for example, you need to know whether the technology you are using is simply capturing “quality codes” or real clinical values. You want to diversify your mix of technologies both because it’s smart and to avoid shortchanging your initiatives. Consider these unique differences among various health care technologies:
- The EMR excels at point of care, gathering clinical information, reminding about prevention and necessary tests, tracking patients awaiting results. But there are weaknesses when more than one EMR is involved in a network or system comparing results across providers, and when the EMR is asked to do true performance measurement and manage complex performance improvement.
- The Health Information Exchange (HIE) can create a faster path to connectivity between EMRs. Its weakness: this is not always easy, doable or economical. Further, the data are not audited for use in analytics or performance measurement, so the HIE’s best use is always checking for tests prior to procedures and at point of care, allowing for validation at that point as well.
- Analytics solutions can answer many questions about volume, trends and some performance. But unless the performance measurement methodology is sound, you can’t count on Analytics-focused solutions to ensure that you meet payer performance benchmarks. In addition, the data are not always actionable in performance improvement.
- Registries, meaning Clinical Data Registries that collect, audit and measure performance, are the engine for performance measurement and, depending on the Registry products, for research and specific performance improvement projects. They also usually audit and validate data coming from EMRs. But do not expect physicians to use them at point-of-care, because the data is retrospective and providers do not have the bandwidth to be able to go back and forth between EMRs and Registries to focus on protocols.
- Performance Measurement and Improvement technologies require frequent calibration to adjust for changing measures and requirements. As a Registry capturing data from EMRs, we often find out-of-date quality codes or data tied to wrong or out-of-date measures that could hurt providers. Performance measurement from any vendor is just not all the same, because an EMR and a Registry have different purposes. The Registry is designed for Performance Measurement, and the EMR for managing the patient’s clinical condition. To use a Registry at point-of-care also makes no sense. It will never have the same patient management functionality of a good EMR, which is designed to convey information directly at the point of patient visits.
- Data are simply not perfect. Many providers want to buy the idea that data “hooks up” patients and technologies, and that data gives you answers. Not so fast—take a look at some of the issues we frequently find in evaluating data. To really make data actionable, you will need to audit it, test it and add experiments (often leading to more data) to reveal the real story.
Buy a System, and Then What?
Fitting the system to goals is a crucial first step. But there’s another, perhaps even larger issue with technology purchases by providers—magical thinking that the technology will solve the problem. Sorry, but the technology is not the solution! It is just an important tool for a long process of change that often raises more questions than answers.
Let’s consider the example of an ACO that is failing to reach targeted savings. Most ACOs have multiple providers with different systems, sparking a desire to create a big ACO database—a solution that is often expensive, depending on the network and underlying systems. Yet many providers firmly believe that having this database will be the key to getting providers on board. How else will they get the answers as to why providers are failing, and what to do about it?
The problem with this approach is that it is excessive. Not every piece of data is essential to identifying where the ACO is failing. Rather, the answer is easily determined by examining a subset of critical providers, looking at network outflow and attribution, and focusing on high-risk patients or high volume providers and specialties.
Taking a different approach by “borrowing” technology from health plans, some ACOs choose to partner with insurers’ technology. After all, they have systems as well as years of experience in medical management, right? The irony here is that insurers have been unsuccessful in holding down costs. What makes us think their technology could work now?
Other ACOs have taken yet another tack: Let’s just build or buy a Health Information Exchange so that we can coordinate care. Again, however, unless you already have proof that poor coordination of care is driving costs, and what measures of coordination will work to maintain the important parts of the patient relationship, an HIE is hard to justify as a sole purchase. Even if the goal of the HIE is to feed data into a clinical database to compare performance, this solution lacks the step of auditing and validating that data to meet performance measurement needs.
What providers often forget is that changing performance requires changing people—both providers and patients—and the culture of medicine itself. This is a marathon effort, not a sprint. Like any major change, it benefits by a careful approach I like to call “Ready, Aim, Fire”: assess the problem you are trying to solve; select the right technology and processes to target that problem; implement, evaluate and repeat. Going for the big “do-it-all” technology presumes that technology can do all three parts of that process. That is both expensive and unrealistic.
An Economical and Practical Technology Investment Plan
Technology should be cast in a supportive role, customized to the health care system and its network and tailored to the solutions needed to improve performance. Just as your organization needs to establish a plan for quality and improvement, your technology should support a step-by-step approach to identifying and resolving problems that stand in the way of successfully bearing risk. These steps include:
- Collect data selectively across your network.
- Performance improvement does not necessarily require the collection of data from all providers across the network, contrary to population assumptions. Data gathering should be dictated entirely by how the organization will implement its performance program, and whether it is focusing on measurement or improvement, or both. The program can be focused on a narrow or phased path of clinical and cost performance, requiring less source system data. Data collection requires a Registry, a data collection vendor or an HIE, and, regardless of choice, requires the step of auditing, validating and normalizing the data before it is used for performance measurement or improvement.
- Analyze the problem. A few of the tasks that organizations should undertake, and the technology solutions that apply:
- Evaluate CMS Quality Resource and Utilization Reports (QRURs) across the organization. The QRURs are practice- and patient-specific data that show how providers compare with others on the basis of CMS-attributed patients. QRURs are rich in detail and important information about networks; consultations to evaluate this detail will help to focus and prioritize health care system efforts.
- Measure performance using Registry technology. Registry-based performance measurement is the strongest method of auditing and validating data on key indicators. This creates the standard for evaluating results across all source systems, practice groups and providers in the next step.
- Analyze key areas of leakage that are big payer targets: inappropriate hospital admissions, readmissions, emergency room use and outpatient costs. This requires consultation for statistical analysis of data by top-tier clinical analytics teams; ideally, results will be exported into both the Registry and the EMR to direct patient care management as well as performance measurement.
- Analyze aggregate performance across the system and compare regional or local differences. This requires Analytics capability that could be built locally on data provided by the Registry, or provided by the Registry itself, or fed to an Analytics vendor.
- Establish ongoing initiatives to address the issues, which will involve process and care design, facilitated by technology.
- Select clinical areas for clinical outcomes improvement, and establish discrete performance improvement projects. Technology must be able to manage the inclusion or exclusion of patient populations, as well as track all provider actions (with any EMR).
- Give analytics and feedback loops to providers, usually provided via a Registry.
- Undertake experiments to determine what is effective or not, which will generally require a Clinical Data Registry that performs or collaborates in research.
The all-in-one technology that miraculously solves all our problems is a seductive dream, sought after by consumers as well as businesses. But at this point in time, that quest remains futile. Improving health care performance is a complex process that requires special functionality to successfully execute distinct steps. Time is too short and resources are too dear to waste on the Fire before Aim.
Founded in 2002, ICLOPS has pioneered data registry solutions for improving patient health. Our industry experts provide comprehensive Solutions that help you both report and improve your performance. ICLOPS is a CMS Qualified Clinical Data Registry.
Contact ICLOPS for a Discovery Session.
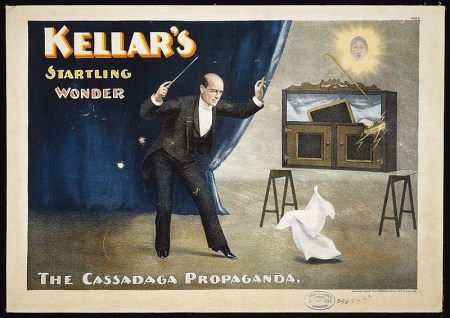
Image Credit: “Kellar’s Startling Wonder: The Cassadaga propaganda,” (Cincinnati, New York: Strobridge Lith. Co., c1894), Library of Congress Magic poster collection.






