We are already more than halfway through the initial year of Medicare’s new Quality Payment Program, which includes MIPS and APMs. Yet already we are seeing some changes from the new administration that will relax requirements for providers, eliminating the need for some to participate and making quality reporting, in particular, easier.
Regardless of how Medicare plays these rules, top providers should maintain a strong strategic focus on Value-Based Health Care initiatives that emphasize performance improvement in cost and quality. Even as Medicare may step back from the leadership role it has taken in this arena, private insurance and employers still consider VBHC the top solution for getting the most value for the health care dollar.
How will the Proposed Rule for Year 2 of the Quality Payment Program affect you? Here’s what you need to know:
1. Participation methods are largely unchanged, but more flexible (especially MIPS APMs).
There are still two tracks for success (MIPS and APMs), and for those participating in MIPS, you still have the option to report individually or as a group, and to do so through a third-party intermediary (such as a QCDR or Registry). Additional proposals continue to promote flexibility, allowing groups to submit QCDR and EHR measures for their Quality score.
If you are in an Alternate Payment Model (APM) that doesn’t meet the Advanced Alternate Payment Model requirements (for example, Track 1 ACOs or the Oncology Care Model without downside risk), you may still bridge the gap by participating in a MIPS APM. Your MIPS score is partially fulfilled by participation in the APM, but also requires some MIPS-specific efforts. The Proposed Rule would make it easier for MIPS APM participants to fulfill requirements and eliminate some of the existing confusion related to MIPS APM scoring.
2. Increasing the “Low Volume Threshold” will mean fewer individual MIPS-Eligible Clinicians.
In 2018, in addition to the previous exclusions (e.g. clinicians who are new to Medicare), CMS is proposing only to hold clinicians or groups accountable for MIPS if they exceed $90,000 in Medicare Part B allowed charges (this is triple the 2017 amount) or see more than 200 Medicare Part B beneficiaries (double the 2017 volume). As in 2017 (and as was the case in PQRS), a clinician is defined by the individual NPI/TIN combination. However, even if certain clinicians are not MIPS Eligible on their own, they still may want to participate in MIPS, either as a Group Practice or in a new method, called a “Virtual Group” (see #4).
3. There are advantageous reasons to opt in, even if you may not need to (spoiler: bonus points and incentive payments).
Even if you are not MIPS-eligible on your own, there are few reasons to consider going in with your group or creating a Virtual Group:
- Improve your patients’ health. The purpose of this program is to quantify performance in order to improve. While the program is certainly not perfect, if you are not measuring your performance in some other manner, it’s impossible to see whether your actions are having an impact (good or bad) on your patients’ health.
- Earn incentives for year-to-year MIPS improvement. The Proposed Rule has established incentives for improving MIPS Quality and MIPS Cost performance year over year. The catch is that, unless there’s a “year 1” to compare, you can’t improve.
- Get a head start on bonus points for exceptional performance. Bonus points are awarded to small practices and for caring for complex patients. By joining in, you give yourself a head start. The bonus points will help you clear the 15 points needed to avoid penalties and increase your opportunity to earn the 70 points needed to qualify for exceptional performance.
- Enhance competitiveness on Physician Compare website. Data submitted for MIPS may be publically reported, and that includes Quality measures, Improvement Activities and Advancing Care Information. You may choose to sit out this round, but that information will be missing from Physician Compare, which will put you at a competitive disadvantage as patients become familiar with the Physician Compare site and resources.
4. Clinicians may participate in MIPS as part of “Virtual Groups.”
A Virtual Group is a group of clinicians (all of whom must be in practices with 10 or fewer providers) who come together to participate in MIPS as a single entity, even though their practices have separate Tax Identification Numbers.
Those who understand that early participation is the key to demonstrating (and being compensated for) improvement, but who are in a small practice, should consider a Virtual Group. This provides an opportunity to pool resources to partner with a QCDR that can get everyone on board, and then flex its data integration muscle to help you track outcomes for your shared patients and improve performance —even if the clinicians in your Virtual Group use different EHRs.
5. MIPS categories have the same effect on your overall score in 2018—even Cost.
As was the case in 2017, MIPS categories are weighted as follows:
- Quality: 60%
- Cost: 0%
- Improvement Activities: 15%
- Advancing Care Information: 25%
Yes, you read that correctly. Although the Cost category was supposed to represent 10 percent of your 2018 MIPS score, this has been rescinded. However, CMS has requested feedback on whether to include cost or not, knowing that it will be 30 percent in 2019. Why eliminate Cost weighting? CMS plans to eliminate the episodic care measures that were originally planned, and to develop new episodic cost measures. Since there will not be an opportunity for providers to preview their results prior to scoring, CMS will not weigh them.
Nevertheless, there are still cost measures that could be incorporated. If Cost is re-assigned its 10 percent weight (which would bring Quality down to 50 percent of the total score), it will be based on the Per Capita costs for all Medicare Beneficiaries and the Medicare Spending Per Beneficiary (MSPB) measures, which have both been retained.
6. Changes to Quality, Improvement Activities and Advancing Care Information are minor.
- Quality: Reporting requirements remain constant—individuals or group practices must report on six measures, one of which must be an outcome measure, for at least 50 percent of the eligible denominator, and that denominator includes all patients. There are a few new challenges, though. Measures that don’t meet the data completeness requirement will only be worth one point, rather than three. In addition, the proposal limits “topped out” measures to six points. You can make up for this with bonus points for reporting additional high-priority measures (as you can this year) and by earning points for improving from year to year.
- Improvement Activities: Scoring requirements are unchanged: 40 points are required for large groups, and 20 points are required for small ones. Points are earned by completing activities worth either 10 or 20 points. This will still be based on attestation, and, if reporting as a group, a single provider may complete an activity on behalf of the entire group. Participants in Patient-Centered Medical Homes are still exempt from this category (as are CPC+ participants, which is a new provision), but now, at least half of the practices in a TIN must be PCMH certified to exempt the TIN from this category.
- Advancing Care Information: The biggest surprise is that the Proposed Rule still allows clinicians to meet objectives through EHRs that have only been ONC-Certified through the 2014 edition, although those who use exclusively 2015 CEHRT earn bonus points.
7. Reporting to a Clinical Data Registry gets more emphasis.
In the Advancing Care Information category, a subtle, but important change has been proposed: rather than reporting to an Immunization Registry, you may earn additional points by reporting to Clinical Data Registries and Public Health Registries. Clinicians may earn 5 percent per reported registry in the ACI performance score (up to 10 percent), and a 5 percent bonus for each additional registry reported that was not already counted in the performance score.
8. Financial Risk for Medical Homes as APMs will be eased in gradually.
Medical Homes that have been created through the CMS Innovation Center may be considered Advanced Alternative Payment Models, meaning that participants are excused from MIPS, but are still part of the Quality Payment Program. The Proposed Rule walks back some of the previously provisioned financial risk. Rather than an estimated 3 percent of average total Medicare Part A and B revenue in 2018, only 2 percent will be at risk. An additional 1 percent will be added in each consecutive year.
9. It’s time to start thinking about All-Payer APMs.
Although this provision will not come into play until 2019, the Proposed Rule lays the groundwork that will enable providers to become Qualified Participants in Advanced APMs (exempting them from MIPS) by participating in a combination of Medicare and Private Health Plan APMs. For those who want to participate in APMs but do not have the required financial risk thresholds (marginal risk of at least 30 percent , a minimum loss rate that doesn’t exceed 4 percent, and a total risk of at least 3 percent), or who don’t meet the nominal risk standard (at least 8 percent ) on the Medicare side, an All-Payer APM will vastly open your options, and enable you to control your own destiny, without creating different standards of care.
10. This is a Proposed Rule—your voice can shape the Final Rule.
None of this is final, so whether you loathe or like what you see, you have until August 18, 2017, to comment. Submit comments electronically (refer to “CMS-5522-P” in your comment), or in writing (CMS will not accept faxes or phone calls). Please see the Rule for instructions on how to comment in writing:
- Download the Unpublished Version.
- Download the Published Version (scheduled for publication on June 30, 2017).
Founded as ICLOPS in 2002, Roji Health Intelligence guides health care systems, providers and patients on the path to better health through Solutions that help providers improve their value and succeed in Risk. Roji Health Intelligence is a CMS Qualified Clinical Data Registry.
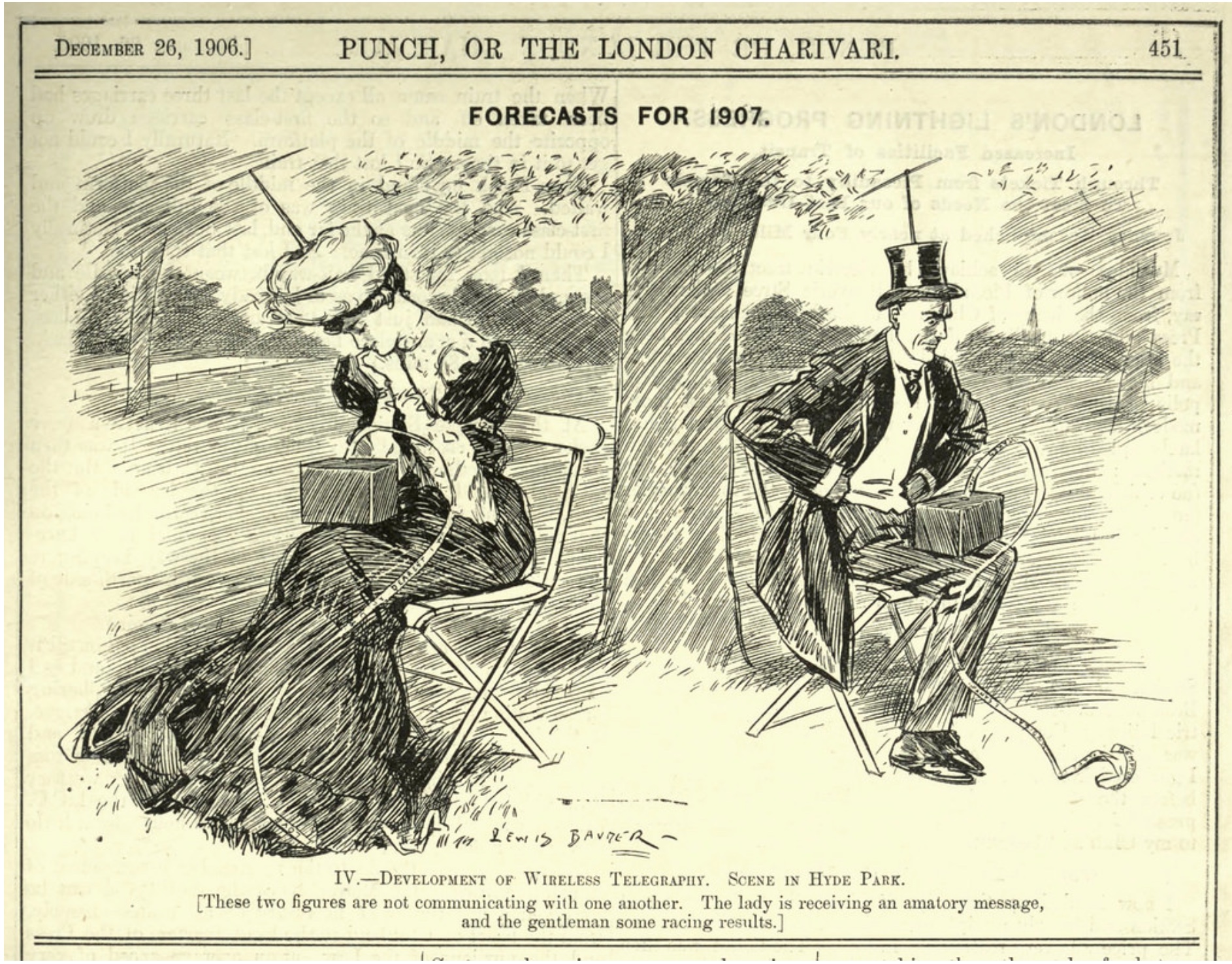
Image Credit: Web Donut